Diabetic Wound Care: How Important is it?
Diabetes is a chronic condition in which the body cannot sufficiently produce or utilize insulin. Up to 1 in 10 Americans are thought to have the disorder, many of whom remain undiagnosed. Diabetes is split into two main sub-types – type 1 and type 2. The former type occurs when the body’s immune system destroys the cells responsible for producing insulin, while the latter occurs when the body cannot produce enough insulin or the body’s cells do react very well to insulin.
If you’ve been diagnosed with type 1 or type 2 diabetes, you’re probably well aware that the condition requires close management and treatment to ensure you avoid dangerous complications and painful symptoms. In this article, we explore the importance of wound care for people with diabetes, as the condition can affect the body’s ability to heal itself. While you may never have experienced issues with wound healing, it’s worth arming yourself with this information. Knowledge is power, after all, and the following facts and tips could help you stay fit, healthy, and thriving long into the future!
Why is Diabetic Wound Care Important?
People with diabetes face a range of complications that can impact their ability to recover from even minor wounds, including:
- Neuropathy (nerve damage): High blood sugar levels can destroy a person’s nerves and render them less sensitive to limb pain (especially in the feet) – a condition known as neuropathy. While lack of pain may seem like a positive thing, patients with neuropathy often fail to notice wounds until weeks or even months after they occurred. Untreated wounds are susceptible to infection and can become more serious over the long term.
- Artery and blood vessel damage: Excessive blood glucose can cause narrowing of the blood vessels and stiffening of the blood vessels. As such, people with diabetes often have circulation problems, affecting the body’s ability to deliver oxygen to wounds and damaged tissue. Without sufficient oxygen, wounds can take a very long to heal.
- Immune system problems: Diabetes can negatively affect immune system function, leaving even minor wounds vulnerable to bacterial infection. If that weren’t bad enough, diabetes also slows down the transportation of white blood cells to damaged tissue. These cells are vital components of the healing response, meaning the wound site will stay open and be susceptible to infection for much longer than it would in people without diabetes. As such, diabetes patients are at higher risk of developing sepsis, gangrene, and osteomyelitis.
The combination of decreased sensitivity to pain and increased risk of infection can mean even minor scratches, cuts, burns, and ulcers can become troublesome problems for people with diabetes. As neuropathy tends to affect the lower limbs, the feet are particularly vulnerable to damage and infection. One of the most serious complications to be aware of is a condition known as Charcot foot.
What is Charcot foot?
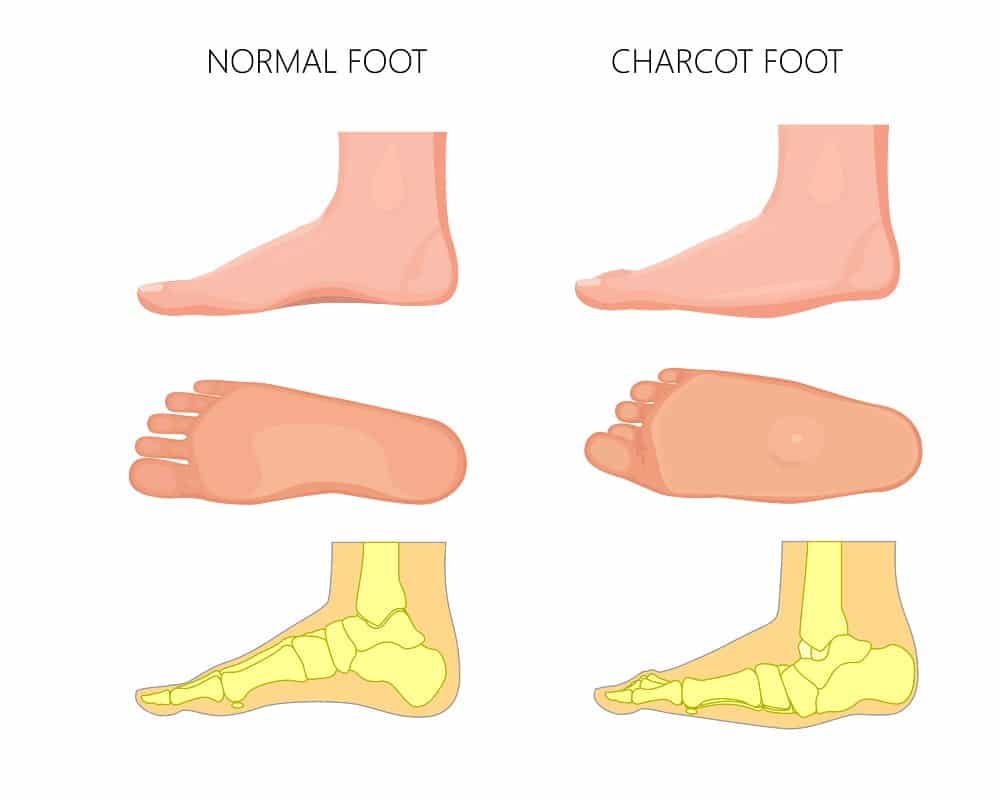
People with neuropathy in their feet often fail to notice injuries or broken bones in the area. Without treatment, these issues can worsen and change the shape of the bones and joints in the feet. Once a person’s foot has changed shape, they are considered to have Charcot foot. In its later stages, Charcot foot can cause ulcers and further deformities. In some cases, infections can become life-threatening and necessitate foot amputation.
What Signs and Symptoms Should I Look Out for?
While Charcot foot may sound scary, rest assured amputations are relatively rare, and you can avoid serious complications by watching out for the following warning signs:
- A change in the color of the foot (people with Charcot foot often find that the skin in the area turns very red).
- Swelling of the foot
- A change in the shape of the foot
- Warmth in the affected area
If you notice one or more of these symptoms, avoid putting too much pressure on your foot and give our office a call immediately. The sooner you ask for help, the lower your chances of developing serious complications. People with diabetes should also check their bodies and especially feet for wounds regularly to avoid infections and potentially life-threatening problems.
When Should I Go to the Podiatrist?
If you’ve been diagnosed with diabetes, we recommend you book a podiatrist appointment at least once a year. Our podiatrists can detect potential problems at an early stage and ensure you don’t suffer the unpleasant consequences of foot ulcers or Charcot foot.
Naturally, you should also visit our office whenever you’re experiencing foot pain or malformations that affect your everyday life. Whether you’re experiencing diabetes-related issues or not, our friendly podiatrists will help you get back on your feet as soon as possible!
Diabetic Wound Care Treatments
The best wound care treatments for people with diabetes are preventative. These include:
- Check your feet every day to spot unusual symptoms or malformations.
- Maintaining a healthy diet and stopping smoking.
- Adhering to any diabetes medication regimens prescribed by your doctor.
- Antibiotic ointments for infected wounds.
- Bandages to protect ulcers and prevent serious infection.
If you end up developing a problem such as Charcot foot, there may be non-surgical options available. These treatments include resting the foot for sustained periods and placing the foot in a protective boot. Once the treatment has run its course, you may be prescribed custom shoes to prevent the development of foot ulcers and allow your bones to heal.
In some cases, you may require surgery. Some surgeries are designed to reshape the foot and move the joints back to their original position. In very rare cases, amputations are required.
Need Help with Diabetic Wound Care? We’ve Got You Covered!
At Richardson Podiatry Center, we understand that diabetes can represent a daunting and worrying diagnosis for many patients. However, you can rest assured we’re here to offer high-quality assistance and treatment to help you maintain an excellent quality of life and prevent foot-related complications. To find out more or make an appointment, reach out today at (972) 690-5374 or fill out a contact form.